This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
This is a case of 50 year old male with shortness of breath and swelling of lower limbs
Patient came to casuality with the chief complaints of shortness of breath since 13 days and swelling of lower limbs since 9 days .
Decreased urine output since 9 days
History of presenting illness :
Patient was apparently asymptomatic 13 days back then he developed
-Shortness of breath which was insidious in onset and progressed to Grade 4 ,aggrevated on lying down and walking and relieved in sitting position.
- He also developed bilateral pedal edema ,since 9 days which is pitting in nature which is insidious in onset and it is initially Grade 1 and presently progressed upto Grade2
-He also had decreased urine output since 9 days.
No history of chest pain,palpitations,syncope,fever, cough,burning micturition and knee pains.
PAST HISTORY:
10 years back -
History of fall from tree
3 years back -
Diagnosed with Tuberculosis and Diabetis mellitus
1 year back -
Noticed swelling in both legs and on consultation was diagnosed with Chronic kidney disease.
-Not a known case of ; Hypertension, thyroid, Asthma
TREATMENT HISTORY:
Drug history:
-NSAIDS intermittently to relieve neck pain
-Antitubercular therapy
- Metformin 500mg three times a day
No history of any surgeries in the past.
PERSONAL HISTORY:-
Diet - mixed
Appetite normal
Sleep - adequate
Bowel - regular;
Micturition : decreased urinary output since 6 days
Addictions - occasionally alcohol consumption
Cigarette stopped 25 years back before 1 pack per year.
Daily routine
He is farmer by occupation and used to go to work by waking up at 6 am and breakfast at 7 am ,completes work by afternoon ,takes rest and has dinner at 8 pm ,sleep at 10pm
He stayed at home since the fall from tree due to low backache
FAMILY HISTORY:-
no significant family history
ALLERGIC HISTORY:-
no allergies to any kind of drugs or food items
GENERAL EXAMINATION:-
Patient is conscious, coherent, and cooperative
Moderately built and well nourished
No pallor
No icterus
No cyanosis
No clubbing
No lymphadenopathy
Pitting edema seen in both lower limbs
VITALS:
Temperature - Afebrile
Pulse Rate - 102 bpm
Respiratory Rate - 15cpm
Blood Pressure - 150/90mmg
Sp02 - 97% at Room air
GRBS - 203 mg/dl
Cvs examination:
INSPECTION:
Shape of chest is normal
Jugular venous pressure is raised
No precordial Bulge
Apical impulse is not well appreciated
No dilated veins.
PALPATION:
Apex Beat - Shifted to 6th intercostal space lateral to mid clavicular line
No parasternal Heave
No thrills
PERCUSSION:
Left border of heart is shifted laterally.
Right border of heart is normal in location
Auscultation :
S1 S2 Heard
RESPIRATORY SYSTEM:
INSPECTION:
-Bilateral Air entry Present
-Trachea is in central position.
-Chest is bilaterally symmetrical and elliptical
-Movements of Chest similar on upper parts
-Expansion of chest is symmetrical in upper part.
PALPATION:
-All inspectory findings confirmed by Palpation
-Tactile vocal fremitus
Right Left
Supra clavicular: normal normal
Infra clavicular: normal normal
Mammary: normal normal
Inframammary normal decreased
Axillary: normal normal
Infra axillary: normal decreased
Supra scapular: normal normal
Infra scapular: normal decreased
Inter scapular: normal normal
Percussion:
Supra clavicular: resonant resonant
Infra clavicular: resonant resonant
Mammary: resonant dull
Axillary: resonant dull
Infra axillary: resonant dull
Supra scapular: resonant resonant
Infra scapular: resonant dull
Inter scapular: resonant dull
ASCULTATION:
-Breath sounds - intensity of breath sounds decreased.
- Vocal resonance
Right. Left
Supra clavicular:. Normal normal
Infra clavicular: Normal Normal
Mammary: Normal Normal
Inframammary: Normal decreased
Axillary: Normal normal
Infra axillary: Normal decreased
Supra scapular: Normal normal
Infra scapular: Normal decreased
Inter scapular: Normal normal
PER ABDOMEN:
INSPECTION
Abdomen is Mildly distended
Umbilicus is central in position
A visible scar due to injury due to a fall around the umbilicus.
PALPATION -
No Tenderness on superficial palapation.
Temperature - Afebrile
Liver is Non Tender and not palpable
Spleen is Not palpable
PERCUSSION: shifting dullness absent
ASCULTATION- Bowel Sounds Heard.
CENTRAL NERVOUS SYSTEM :
Patient is conscious coherent and cooperative
Speech is normal
No signs of meningeal irritation
Cranial nerves - intact
Sensory system normal
Motor system:
Tone - normal
Bulk - normal
Power - bilaterally 5/5
Deep tendon reflexes
Biceps : ++
Triceps : ++
Supinator: ++
Knee : ++
Ankle : ++
Superficial reflexes - normal
Gait - normal
Provisional diagnosis:
heart failure with B/ L Pleural effusion
INVESTIGATIONS:
Hemogram:
Hemoglobin 11.7 gm/dl
Total count 9,000 cells/cumm
Neutrophils. 74
Lymphocytes 20
Eosinophils 2
Monocytes 4
Basophils 0
Pcv. 36.5 vol
Mcv. 82.8 fl
RDW- CV 19.1 %
RBC COUNT:. 4.4 million/cu/mm
LIVER FUNCTION TEST
Total Bilirubin - 0.9 mg/dl
Direct Bilirubin - 0.1 mg/dl
Indirect Bilirubin - 0.8 mg/dl
Alkaline Phosphatase - 221 u/l
AST - 40 u/l
ALT - 81 u/l
Protein Total - 6.8g/dl
Albumin - 4.2 g/dl
Globulin - 2.6 g/dl
Albumin:Globulin Ratio - 1.6
Renal Function Test
Urea - 64
Creatinine - 4.3
Na+ - 138
K+ - 3.4
Cl- - 104
Spot urine Protein - 34
Spot urine creatinine - 14.8
Spot Urine : Creatinine Ratio - 2.29
Fasting Blood Sugar - 93mg/dl
PLBS - 152 mg/dl
HbA1c - 6.5%
ABG :
pH : 7.3
pCO2 - 28.0
pO2 - 77.4
HCO3-.13.5
Spo2-94.7
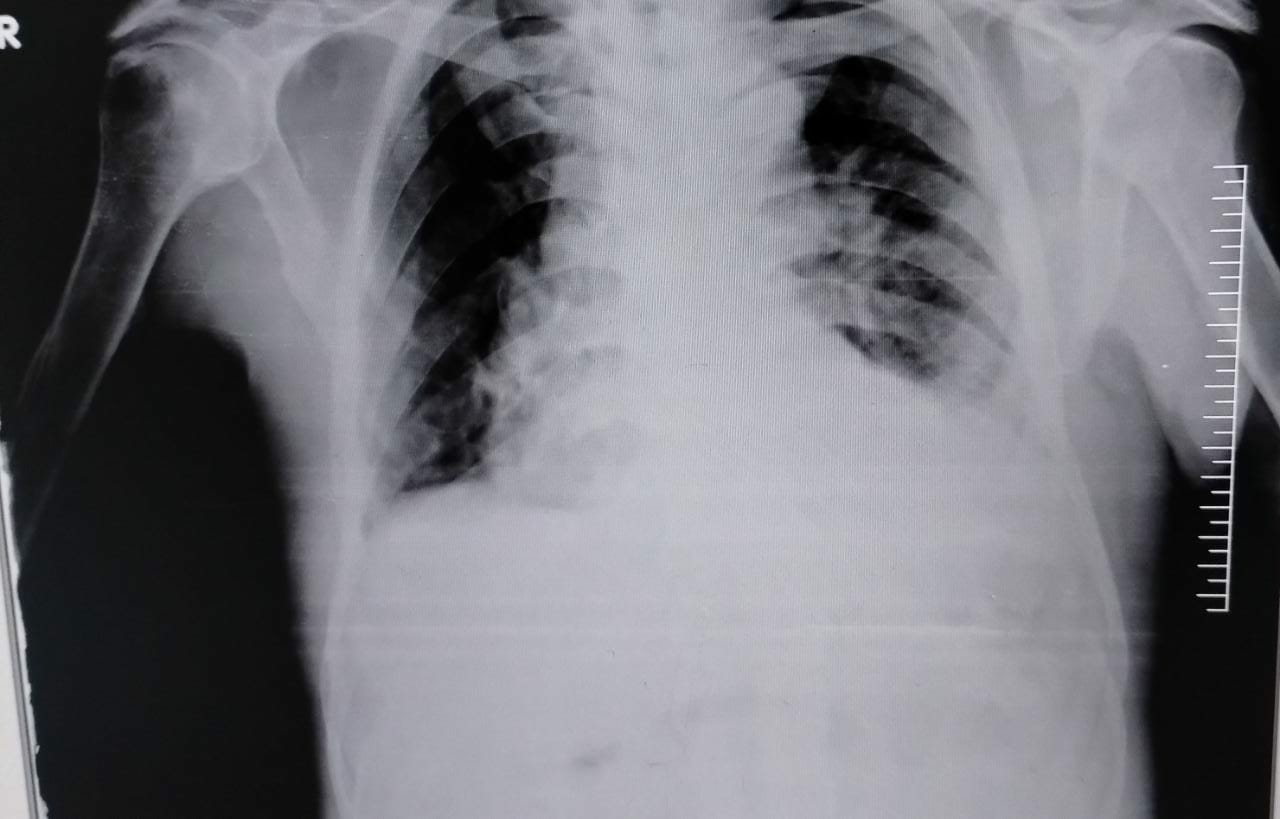
Chest X Ray
2D echo
MODERATE MR+: MODERATE TR+ WITH PAH: TRIVIAL ECCENTRIC TR+
GLOBAL HYPOKINETIC, NO AS/MS. SCLEROTIC
MODERATE LV DYSFUNCTION+
DIASTOLIC DYSFUNCTION PRESENT
ULTRASOUND:
USG CHEST:
IMPRESSION:
BILATERAL PLEURAL EFFUSION (RIGHT MORE THAN LEFT) WITH UNDERLYING COLLAPSE.
USG ABDOMEN AND PELVIS:
MILD TO MODERATE ASCITES
RAISED ECHOGENICITY OF BILATERAL KIDNEYS.
X RAY NECK:
DIAGNOSIS:-
HEART FAILURE WITH reduced EJECTION FRACTION
WITH ACUTE KIDNEY INJURY ON CHRONIC KIDNEY DISEASE (SECONDARY TO DIABETES/NSAID INDUCED)
WITH K/C/O DM II SINCE 3 YEARS
WITh TB 3 years ago
TREATMENT
1)Fluid Restriction less than 1.5 Lit/day
2) Salt restriction less than 1.2gm/day
3) INJ. Lasix 40mg IV / BD
4) TAB MET XL 25 mg
5) TAB. CINOD 5 MG PO/OD(IF SBP MORE THAN 110 MM HG)
6. INJ. HUMAN ACTRAPID INSULIN SC/TID (ACCORDING TO SLIDING SCALE)
7. INJ. PAN 40 MG IV/OD
8. INJ. ZOFER 4 MG IV/SOS
9. Strict I/O Charting
10. Vitals Monitoring
11. TAB. ECOSPRIN AV 75/10 MG PO/












Comments
Post a Comment