A 71 year old male patient with the cheif complaints of weakness in right upper limb
"This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient - centered online learning portfolio and your valuable inputs on the comment"
71 year old male came to hospital with chief complaints of weakness in right upper limb since 4 days and slurring of speech since 3 days
HOPI: patient is known case of cerebrovascular accident
1 year back associated with bilateral upper limb
weakness he was given medications and sent back
He used the medication for about 5 months and then
Stopped taking drugs.
5 years back he gives history of chest pain squeezing type and , he was admitted to the
Hospital PTCA was done to manage the patient.
3 days back he woke up from sleep and noticed
Numbness and tingling sensations in the both hands ,
He noticed that he was unable to eat the food with hand,
He was not able to make fist , weakness in lifting the
Right hand
From 2 days he has slurring of speech
He has no H/o fever, trauma , nausea, vomiting,infections, seizures ,loss of consciousness
Daily activities: he used to wake up by 6 o clock in the
Morning,used to complete daily activities
Past History : No History of diabetes, hypertension seizures, asthma, TB ,
Personal history: DIET: Mixed
Appetite : normal
Bowel and bladder movements : regular
Sleep : inadequate
Addictions: chronic beedi smoker for about 40 yrs
Occasionally consumes alcohol
Family History: not Significant
Treatment history : he was taking lipid lowering and anti platelet drugs and stopped 5 months back
Surgical history: he was treated with minimally invasive procedure PTCA about 5 years back.
General Examination:
Patient is Conscious, Cooperative and is oriented to time, Place and Person.
He is moderately Built and Nourished
.
Pallor :Absent
Icterus: Absent
Clubbing : present
Cyanosis :Absent
Lymphadenopathy :Absent
Edema:Absent
Vitals :
Temperature - afebrile
Pulse- 90 bpm
B.P -110/80 mm Hg
RR - 18 cpm
SYSTEMIC EXAMINATION :
CVS : S1 S2 heard, no murmurs
RS : Bilateral air entry present, normal vesicular breath sounds, no added sounds
GIT : Soft, non-tender, no organomegaly
CNS EXAMINATION:
Dominance - Right handed
Higher mental functions
• conscious
• oriented to person and place
• memory - able to recognize their family members
Patient is emotionally stable and his behaviour and appearance is appropriate
Slurring of speech is present
Recent immediate and remote memory is intact
Cranial nerve examination
• 1 - normal
• 2- Direct and indirect light reflex present
- Rt - No perception of light. Non reactive pupil.
Extraocular movemts are normal
Lt - Light reflex is present. He is able to count fingers at 6 m
• 3,4,6 - no ptosis Or nystagmus
• 5- corneal reflex present
• 7- slight deviation of mouth, loss of nasolabial folds, forehead wrinkling present
• 8- able to hear
• 9,10- normal
• 11- sternocleidomastoid contraction present
•12 - no tongue deviation
Motor system :
Attitude -
Tone - normal tone on right side(both UL,LL)
Normal tone on left side(UL,LL)
Power:
Right Left
UL 3/5 4/5
LL. 4/5 4/5
Reflexes : superficial reflexes : corneal reflex, conjunctival reflex, abdominal reflex , plantar reflex present
On both sides,
Right left
Biceps 2 + 2+
Triceps 2 + 2+
Knee jerk 2+ 2+
Ankle jerk . 1+ 1+
Supinator 2+ 2+
Sensory examination:
Crude touch : normal
Pain: normal
Temperature: normal
Fine touch : normal
2 point discrimination: normal
Stereognosis: normal
Cerebellar signs :
Knee heel test, finger nose test , dysdiadokokinesia
All test findings are normal.
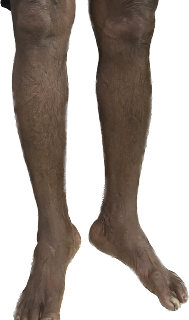
Clinical pictures
Investigations: ECG :
Provisional diagnosis: recurrent cerebrovascular accident?
Treatment : iv fluids
Tab ecosprin
Lactulose
Tab pantaprazole
Tab Atorvastat












Comments
Post a Comment