A 70 year old female with shortness of breath
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
A 70 year old female came to opd with the chief complaints of shortness of breath since 10 days,fever since 10 days ,burning micturition and decreased urine output since 4 days , loss of appetite since 6 days,
HOPI : patient was alright 11 days back then she developed fever which is insidious in onset ,high grade,intermittent in nature associated with chills and rigor and it releived on taking medication .she is having shortness of breath grade 4 since 10 days,it aggravated 3 days back ,patient also complains of burning micturition and decreased urine output since 5 days
patient gives a history of diabetes mellitus from the past 15 years ,hypertension from 10 years ,she is taking medications tab metformin 500 mg po/od,tab telma 40 12.5 mg po/od, patient was taken to hospital 9 days back,and there diagnosis of typhoid was made and treatment was given
past history: K/C/O DM from 15 years
HTN Since 10 years
patient is not a k/c/o TB ,ASTHMA,CAD,EPILEPSY.
personal History:
She consumes mixed diet
Appetite is decreased in the past 6 days
Sleep is adequate
Bowel regular and decrease in urine output.
No addictions.
Family history: no significant family history
GENERAL PHYSICAL EXAMINATION: patient is conscious, coherent,cooperative well oriented to time ,place and person .she is obese and moderately nourished.
pallor present
icterus absent
clubbing absent
cyanosis absent
lympadenopathy absent
edema present
PROVISIONAL DIAGNOSIS
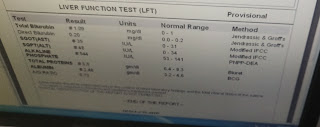
AKI on CKD
TREATMENT
Rx
Head End Elevation upto 30°
Inj PIPTAZ 2.25 gram IV/ BD
Inj. Neomal 1gm Iv SOS if temp > 101F
T. Lasix 40mg PO/BD if SBP> 110mm hg
T. Nodosis 500 mg. PO/ TID
T. Orofer XT PO/ OD
T. Shelcal 500 mg PO/OD
T. PCM 500 mg PO /SOS
Cap Bio D3 PO / weekly twice.
BP monitoring every 2 hours
Fever charting every 6 hours
Vitals monitoring every 4th hourly.














Comments
Post a Comment