A 50 YEAR OLD WOMAN WITH SOB,ODYNOPHAGIA
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
A 50 year old woman came to OPD with chief complaints of shortness of breath ( grade 2) since 20 days ,difficulty in swallowing both solids and liquids since 4 days .
HISTORY OF PRESENT ILLNESS:
Patient was apparently alright 10 yrs ago and went to Hospital in view of headache, easy fatigability and was diagnosed with hypertension and started on medications
6 years ago hospital in view of weight gain and easy fatigability and was diagnosed with Hypothyroidism and is using Thyronorm 50mcg
Later was diagnosed with Rheumatoid arthritis but is not on any medication
3 months ago diagnosed with DM and is not in medication
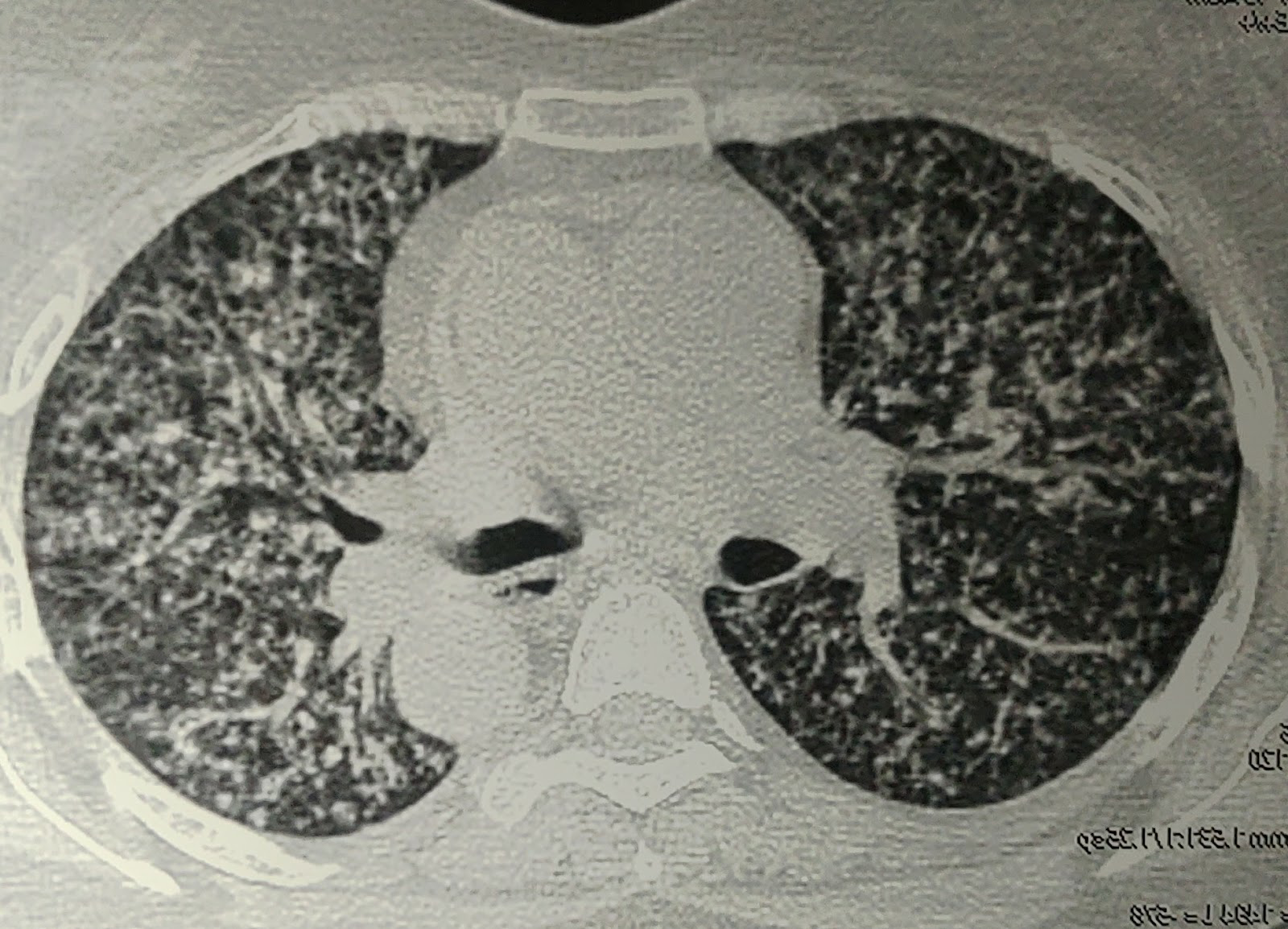
2 months back pt had c/o cough with expectoration, pain in chest region. Was diagnosed as PULMONARY MILIARY TB and started ATT. After 1 month of use she started developing redness and itching all over the body, ATT induced Erythroderma, stopped ATT (1-2-22) for 20 days and again started using 20 days back
20days back after being discharged from a hospital admitted for ATT induced Erythroderma. She is having SOB (grade 2), not associated with any orthopnea/PND, pedal Edema, chest pain, or palpitations.
From 4 days she is having difficulty in swallowing solids and liquids and from 2 daya she is not able to open her mouth because of pain and c/o reddish discolouration of the tongue.
PAST HISTORY: she is a k/c/o HTN since 10 years (on medication)
Hypothyroidism since 6 years ( on thyronorm 50 mcg
DM since 3 months( not on medication)
k/c/o of miliary TB and she is on ATT ( HRZE), she is also suffering from rheumatoid arthritis
PERSONAL HISTORY:
DIET:mixed
APPETITE: good
BOWEL AND BLADDER MOVEMENTS:regulat
SLEEP: not adequate
ADDICTIONS :no addictions
FAMILY HISTORY: no significant family history















Comments
Post a Comment